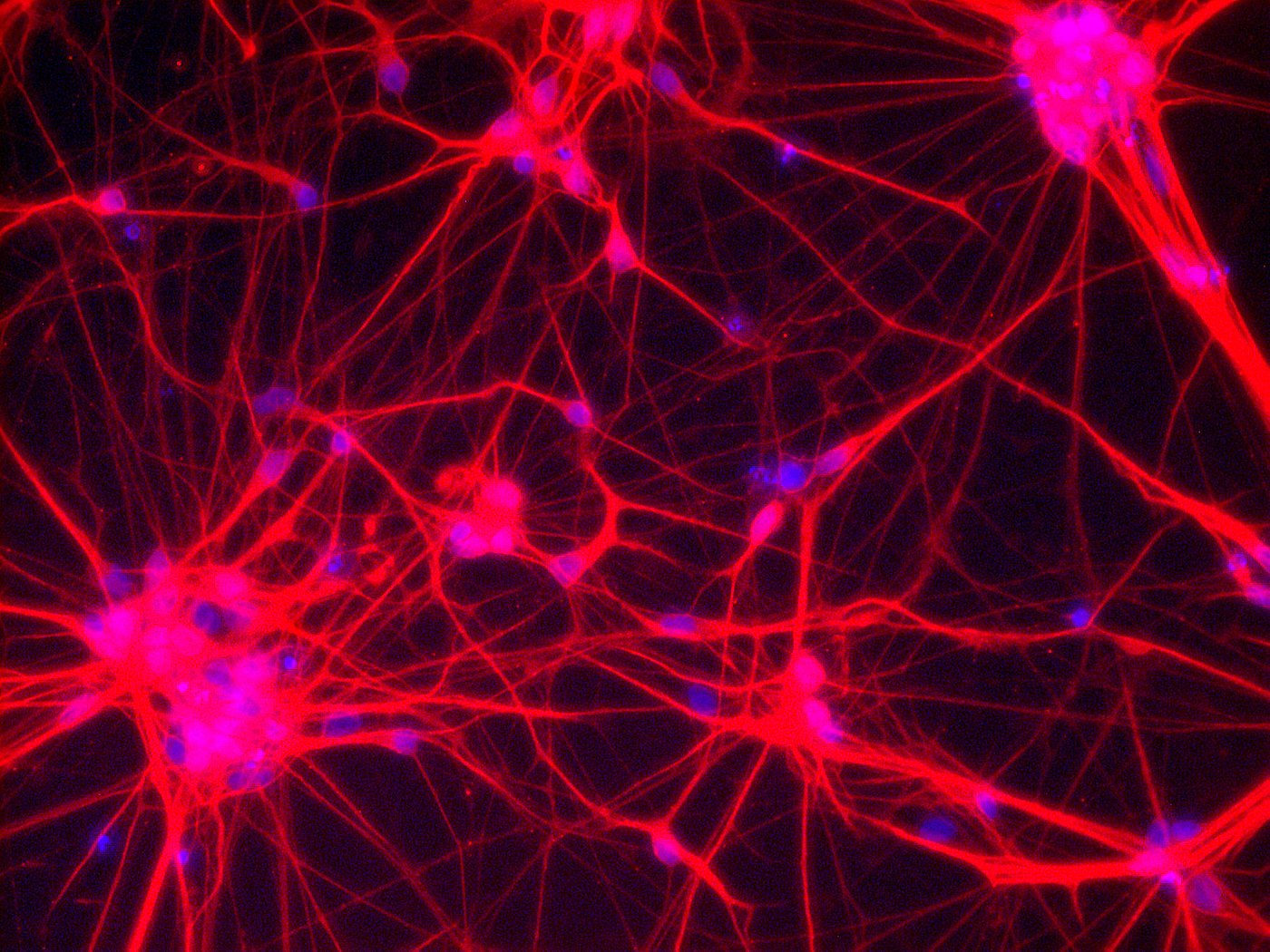
Neurons – Network of neuronal cells (Blue: nucleus; Red: neurons) [Copyright: Institute for Transfusion Medicine, UK Essen]
Parkinson’s disease is the second most common neurodegenerative disease and more than 6 million people worldwide are affected. The cause of Parkinson’s disease (named after an English doctor called James Parkinson) is still unknown, but it is believed that genetic as well as environmental factors play a role. Characteristic of Parkinson’s disease is the loss of dopaminergic neurons, a highly specialized type of neuron in the brain which produces the neurotransmitter dopamine. Loss of dopaminergic neurons causes the typical movement-related symptoms (e.g. trembling, difficulty walking). In addition to movement-related symptoms, other symptoms like neuropsychiatric problems (e.g. mood, cognition, and behavior) as well as sleep difficulties, dementia, and depression might occur.
Unfortunately there is no cure for Parkinson’s disease yet, only treatments to address the symptoms. However, a very promising source are human pluripotent stem cells. If it were possible to replace dead dopamine-making neurons in people with Parkinson’s, this could potentially stop disease progression or even reverse it. Researchers have been working for decades on this approach, either using embryonic stem cells or reprogrammed adult somatic cells to produce dopaminergic neurons.
Stem cells could open new opportunities to treat Parkinson’s disease
Now the first-in-human clinical trial using induced pluripotent stem (iPS) cells to treat Parkinson’s disease just started this August in Japan and will recruit a total of seven patients. The approach of the team around Jun Takahashi, a neurosurgeon at Kyoto University’s Center for iPS Cell Research and Application (CiRA), is to derive dopaminergic progenitor cells from iPS cells and then perform neurosurgery to inject the reprogrammed cells into the putamen, a round structure located at the base of the forebrain. Two small holes will be drilled into the patients’ skulls to be able to inject about 5 million cells. Since the transplanted neurons must mature and create millions of connections in the brain, the first benefits of the treatment are expected six months or later after surgery. However, in contrast to medication it is hoped that via a single treatment a lifelong benefit will be achieved, because the cells should stably engraft and then can produce dopamine in situ.
Theoretically it would even be possible to create patient-specific (autologous) iPS cells, but producing customized iPS cells would be expensive and it can take a couple of months to derive and grow the cells. Therefore researchers decided to use stocks of iPS cells from healthy donors that are less likely to cause immune rejection. However, patients will still receive a common immunosuppressant drug as a precaution.
Prior studies showed promising results
Before an approach is tested in humans, many preclinical studies are conducted to obtain a proof-of-principle. The Japanese team has previously tested the same trial strategy in macaque monkeys (reported in our newsletter 04/2017): neurons prepared from human iPS cells were injected into the monkeys’ brains and implanted cells survived there for at least two years without causing any dangerous effects (e.g. development of tumors). Moreover, the transplanted neurons formed connections with the monkeys’ brain cells. A significant movement improvement lasting two years after surgery was observed. The next step is then to perform a clinical trial to find out whether the results from animal models can be translated to humans, as the real proof of treatment can only be achieved with affected patients.
Research efforts all over the world
Not only in Japan have researchers been working for years on the development of stem-cell-based treatments for Parkinson’s disease. Leading researchers from the field (including Jun Takahashi) who share common therapeutic ambitions have formed a consortium called “GForce-PD” to jointly bring approaches to the clinic. Lorenz Studer from the Sloan Kettering Institute in New York, who has been working on Parkinson’s disease for more than 20 years, recently stated that a clinical trial will start soon, but in contrast to Jun Takahashi’s trial he will transplant dopamine-producing neurons derived from embryonic stem cells. The trial will probably be a combined phase I/IIa study, based on an approach tested before in mice, rats, and monkeys. Results of the ongoing clinical trial in Japan and further planned trials with embryonic stem cells are awaited in two to three years, and will most likely be followed by phase II and phase III studies. However, the major goal of a phase I clinical trial is to show that the approach is feasible and safe.
It was reported that researchers in Australia and China (who are not part of GForce-PD) already started a clinical trial injecting neuronal-precursor cells derived from embryonic stem cells into the brains of Parkinson’s patients. However, researchers from the GForce-PD consortium expressed safety concerns about this approach because neural precursor cells are used, which are still able to differentiate into neurons other than the desired kind and might accumulate dangerous mutations. Furthermore, there is apparently no peer-reviewed preclinical data on these approaches available.
Stem cell-based treatments for neurodegenerative disease
Cell replacement therapy for Parkinson’s disease is a very promising approach. A new and exciting era has started with the first iPS-cells-based clinical trial in Japan, even though it will still take several years for the market authorization of a stem cell-based treatment for Parkinson’s disease. However, these clinical trials are pioneering and will help to develop new cell-based treatments for Parkinson’s disease, which will hopefully pave the way for further stem-cell-based therapies to treat other neurological disorders.
Further reading:
Further information: