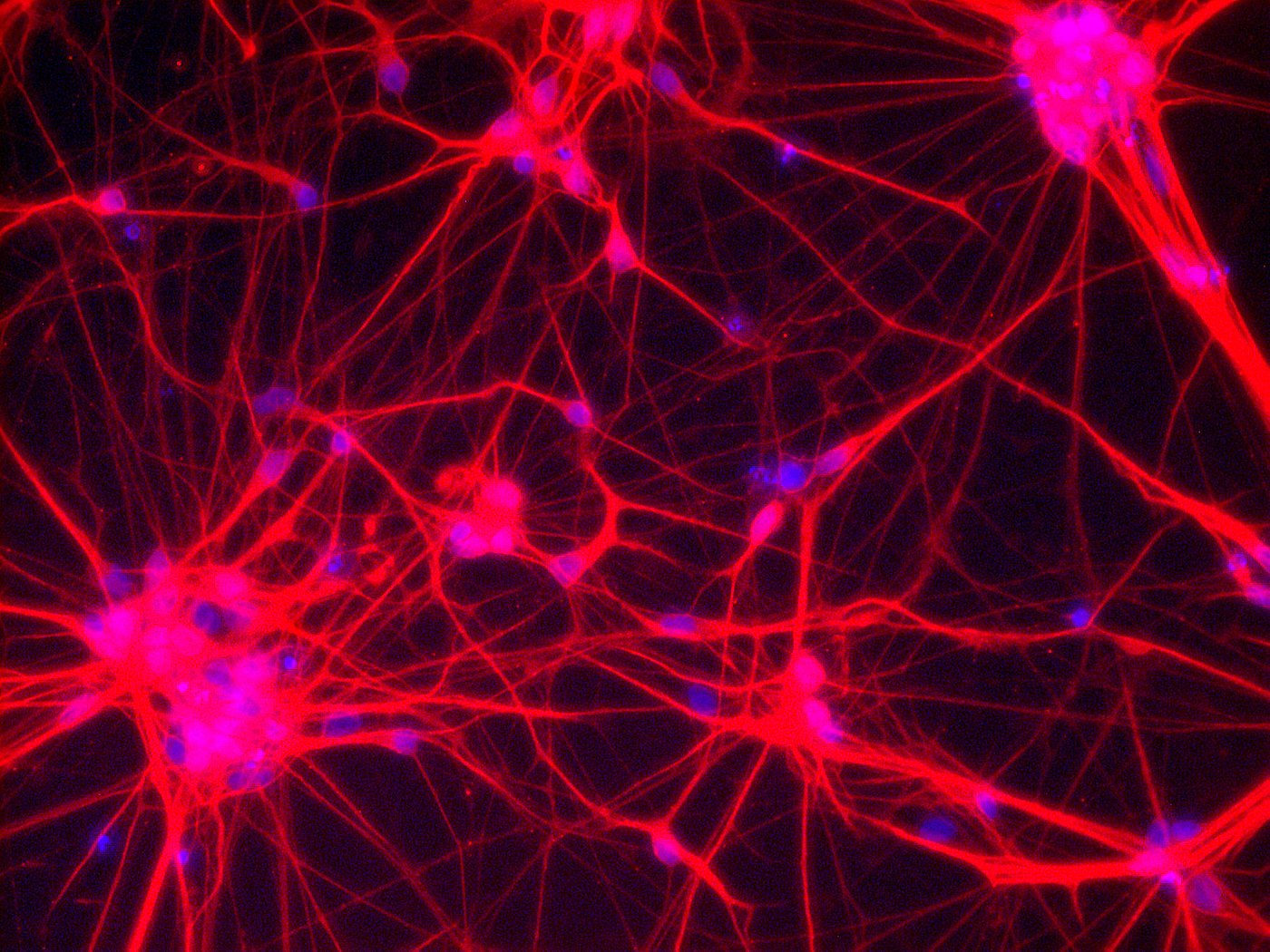
Neurons – Network of neuronal cells (Blue: nucleus; Red: neurons) [Copyright: Institute for Transfusion Medicine, UK Essen]
Translational stem cell research projects bridge the gap between fundamental research carried out in the lab and the application of this research to the field of patient care.
Who are the people behind these kinds of projects? What interests them - in their own research field, but also above and beyond it? What drives them right now?
The aim of this series is to try and make the abstract term ‘translation’ more tangible and to give a glimpse behind the scenes of the world of translational stem cell research. Part two of the series introduces Dr. Nina Neuhaus from Münster.
I am … About me in brief: my name is Nina Neuhaus. I am 36 years old and I am a biologist. I am married and the mother of a two-year old daughter. I work at the Centre of Reproductive Medicine and Andrology (CeRA). A distinguishing feature of this center is that both scientists engaged in basic research and clinicians work together to investigate issues related to male reproduction in multidisciplinary teams.
My research at CeRA is focused on the human spermatogonial stem cells of the testicles, which are responsible for sperm production from puberty onwards. In my view, studies of this kind which investigate the potential of these stem cells as a fertility reserve are vital. The reason being that specialized centers worldwide have begun to store the immature testis tissue of child patients who are exposed to a high risk of being confronted with subfertility or infertility in the future due to a forthcoming cancer treatment. Prior to gonadotoxic treatment, adult males have the option of cryopreserving sperm as a fertility reserve, which can then be used at a later date as part of artificial insemination. However, this approach is only possible for patients after the onset of puberty and the associated begin of sperm production. For pre-pubescent and peri-pubescent patients, the undifferentiated spermatogonial stem cells in testis tissue are the only option. As a result, the risk of permanent fertility loss presents a particular burden for these boys.
Professor Stefan Schlatt, Director of CeRA at the University of Münster, and Professor Sabine Kliesch, Head of Clinical and Operative Andrology, have set up the initiative 'Androprotect' as they are determined to provide even pre-pubescent boys with the opportunity of fatherhood at a later date. The aim of this clinical network is to establish a national tissue bank based in Münster which serves the whole of Germany, in order to preserve the testis tissue of these pre-pubescent patients (and thus also their stem cells). At the moment however there are no validated protocols for differentiating spermatogonial stem cells in sperm in vitro to ultimately enable these patients to have their own biological children. As these patients will be presenting for fertility treatment within the next 10-20 years, there is an urgent need for research in this area. Thanks to the funding for our project 'Testicular Stem Cells: Innovative Treatment Options for Preserving Fertility in Pre-Pubescent Boys with Germ Cell Defects' awarded as part of the Translational Stem Cell Research funding competition, we have been able to drive the research forward in this field. More precisely, in the last few years it has been possible to demonstrate (using a mouse model) that the differentiation of spermatogonial stem cells in fertile sperm can be achieved using organ cultures (Sato et al., Nature, 2011). The publication of this study in Nature represented a breakthrough in our research field. However, the stem cell systems of testicles differ greatly between rodents and primates, including humans. Thus further modifications to the protocols are necessary in order to be able to achieve in vitro spermatogenesis in humans.
What importance does the funding from the call ‚Translational Stem Cell Research’ have for you personally and for your work in general? This funding was hugely important for me personally and also for CeRA as it gave us the opportunity for the first time to carry out urgently needed translational analyses. Thanks to the funding we were able to evaluate immature testis tissue in terms of the number of stem cells and their degree of differentiation. At the same time, we were able to carry out initial in vitro cultures by using a non-human primate model in order to determine the factors necessary for a successful differentiation of stem cells in sperm. To summarize, this funding has enabled us to establish evaluation categories for previously stored and future immature testicle samples which describe the potential of each tissue sample as a fertility reserve. The first translation of findings to the clinic has already taken place, as the new evaluation categories are to be included in the patients´ results. Furthermore, the data generated will form the basis for a scientific publication in the field of translational research and also for future research applications.
A scientific highlight for me right now ... Since the 1960s, researchers have tried to differentiate spermatogonial stems cells in the model system and in humans. In recent years, this has finally been achieved in rodent models and the culture systems have continued to improve. In particular, it was possible to improve the supply of nutrients to the tissue with a combination of microfluid systems. Using these new approaches, we are attempting to achieve in vitro spermatogenesis with human material in the new future.
What I would also like to achieve this month outside of the world of science ... Have a crazy kid's party to celebrate my daughter's third birthday!